NCI trial leads to first drug approval for a very rare cancer.

When Tesu Kim had surgery to remove a mass in his leg that wouldn’t stop growing, doctors told him he had alveolar soft part sarcoma (ASPS). He would need further treatment to keep the cancer under control. The NIH Clinical Center made the experience as easy as possible, he recalls, treating him kindly and providing transportation from his home in Columbia, Maryland. When the initial medications they gave him stopped working, he was invited to join a clinical trial investigating atezolizumab’s ability to stop the rare cancer. The new drug not only kept his tumors in check but shrank them, and it caused none of the side effects he’d experienced with his previous treatment. Five years later, he remains on atezolizumab, and his cancer remains stable. He fits in regular visits to the Clinical Center in between work and classes at Howard Community College, and he even finds time for vacations. Here he is on a trip to Dubai in June 2023, having a unique dining experience about 150 feet up in the air at “Dinner in the Sky.” Credit: Tesu Kim
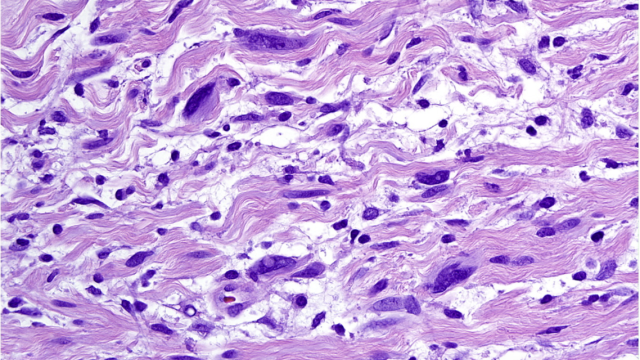
Alveolar soft part sarcoma (ASPS) is a slow-growing cancer that starts in soft tissues. It is diagnosed in fewer than 100 people each year in the United States, most of whom are adolescents and young adults. ASPS does not respond to chemotherapy, and when patients’ tumors cannot be removed surgically, it has been difficult to treat.
Many patients with ASPS are referred to the NIH Clinical Center, where a clinical trial recently led to the first FDA-approved treatment for advanced cases of the cancer.
Encouraged both by laboratory findings and reports of a few patients with ASPS who had improved following treatment with a type of immunotherapy called checkpoint inhibitors, Alice Chen, M.D., Head of the Developmental Therapeutics Clinic in NCI’s Division of Cancer Treatment and Diagnosis (DCTD), considered the use of the immunotherapy atezolizumab as an effective treatment for ASPS. So, Chen and her team launched a clinical trial.
The results of the trial, which was conducted at the NIH Clinical Center and at sites in the NCI’s Experimental Therapeutics Clinical Trials Network, were reported in the New England Journal of Medicine. For 19 of the 52 participants, tumors shrank by at least 30 percent following treatment with atezolizumab. Most other patients were considered to have stable disease, meaning their tumors were not growing or shrinking.
The side effects of atezolizumab were mostly mild, and the treatment was generally well tolerated by patients. “I think we've made an impact for a majority of these patients’ lives,” says Chen. “They were able to continue to do their daily living.”
A collaboration with researchers in CCR’s Pediatric Oncology Branch, led by Associate Research Physician John Glod, M.D., Ph.D., enabled children as young as two to participate in the trial. Glod says that approach is crucial for advancing treatment options for children with very rare cancers like ASPS. “There just aren't enough pediatric patients to do a standalone study,” he says, “so this is a way we can make more rapid progress for kids.”
Tumor biopsies collected during the trial enabled the research team to investigate changes brought about by the treatment. Their findings suggest atezolizumab enabled patients’ immune systems to attack their tumors as intended. “For many of the patients who had an objective shrinkage in their tumor after treatment, we could show that not only was the tumor now infiltrated with more T cells, the T-cell killing apparatus was activated,” says DCTD director and CCR Senior Investigator James Doroshow, M.D.
James H. Doroshow, M.D.
Senior Investigator
Developmental Therapeutics Branch
Deputy Director
Clinical and Translational Research, NCI
Alice Chen, M.D.
Head
Early Clinical Trials Development Program and the Development Therapeutics Clinic, NCI
John W. Glod, M.D., Ph.D.
Associate Research Physician
Pediatric Oncology Branch
Based on early reports from the trial, the FDA approved atezolizumab for adults and children with ASPS in 2022. It is the first pediatric approval of atezolizumab for any disease. The scientists stress that the success is the result of cooperation between DCTD, the CCR Pediatric Oncology Branch, the Experimental Therapeutics Clinical Trials Network and Genentech, a member of the Roche Group, which provided the drug through a cooperative research and development agreement with NCI.