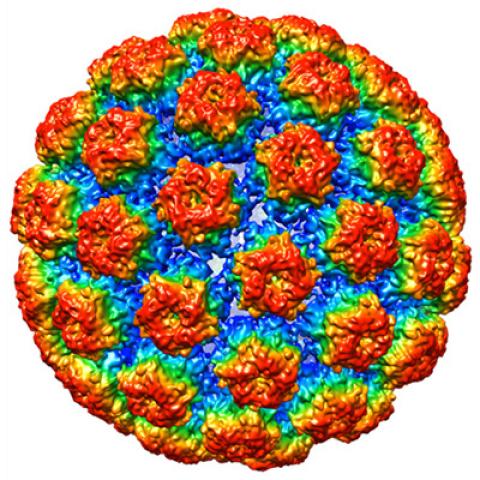
The structure of HPV 16.
Photo courtesy of Christopher Buck
Scientists at NCI’s Center for Cancer Research are launching a phase II clinical trial to evaluate the effect of a single immunotherapy treatment on precancerous lesions that put women at risk for vulvar cancer. Like the cell-based immunotherapies now used to treat certain blood cancers, the experimental treatment aims to use patients’ own immune cells to fight disease. In this case, patients’ T cells will be reprogrammed in the laboratory to find and eliminate cells that have been infected with the human papillomavirus (HPV), a virus that contributes to several types of cancer, including vulvar cancer.
The trial, led by Christian S. Hinrichs, M.D., an Investigator in the Experimental Transplantation and Immunology Branch, is open to women with vulvar high-grade squamous intraepithelial lesions (HSIL), a rare condition caused by chronic infection with HPV. Women with the condition develop lesions on the outer surface of the vulva, the area of skin that surrounds the urethra, vagina, clitoris and labia. These lesions, which can be itchy or painful, rarely go away on their own and can become cancerous. They are usually removed surgically, which in some cases can damage nearby parts of the patient’s anatomy and impair function. Because the HPV infection remains after treatment, many patients develop new lesions and may need additional surgeries.
The experimental cell-based immunotherapy, developed in Dr. Hinrichs’ laboratory, is a systemic treatment that aims to combat both the HPV infection and vulvar HSIL. Hinrichs’ team has been working to develop cellular immunotherapies against HPV-related cancers and recently discovered a receptor that effectively directs T cells to attack HPV-infected cells. To enhance the immune system’s defenses against the virus, the research team will collect T cells from each study participant’s blood and genetically modify the cells to produce that receptor, which targets a viral protein called E7 that signals HPV infection. The E7-targeting T cells will then be administered to patients by infusion during a brief in-patient stay at the NIH Clinical Center in Bethesda, Md.
Following the infusion, the modified T cells are expected to multiply and circulate throughout the patient’s body to fight the infection. Patients will be monitored to assess the treatment’s effects on the virus and determine whether precancerous vulvar lesions go away or get smaller. There is no cost to study participants for treatment or follow-up at NIH.
The trial will be the first to test whether engineered T cells can help the body eliminate precancerous HPV-related disease. In 2018, Hinrichs and colleagues tested the effects of T cells with the same E7 receptor in a small phase I clinical trial involving patients with HPV-associated cancers. The treatment was found to be safe, and some patients experienced regression of their tumors.
Although this clinical trial is designed to evaluate the treatment’s effects on vulvar HSIL, Hinrichs says the same approach might also be useful toward premalignant HPV infections associated with other cancers, including cervical and anal cancers.
The initial stage of the trial will include 12 women with vulvar HSIL who are not considered good candidates for surgical management of the condition.
Clinicaltrials.gov identifier: NCT03937791
NCI Protocol ID: 19-C-0091
Official Title: Immunotherapy with E7 T Cell Receptor T Cells for Vulvar High-Grade Squamous Intraepithelial Lesions
The Center for Cancer Research is NCI’s internal cancer center, a publicly funded organization working to improve the lives of cancer patients by solving important, challenging and neglected problems in cancer research and patient care. Highly trained physician-scientists develop and carry out clinical trials to create the medicines of tomorrow treating patients at the world’s largest dedicated research hospital on the campus of the National Institutes of Health in Bethesda, Maryland.
For more information on CCR clinical trials click here, and subscribe to have the latest CCR clinical trials sent directly to your inbox.